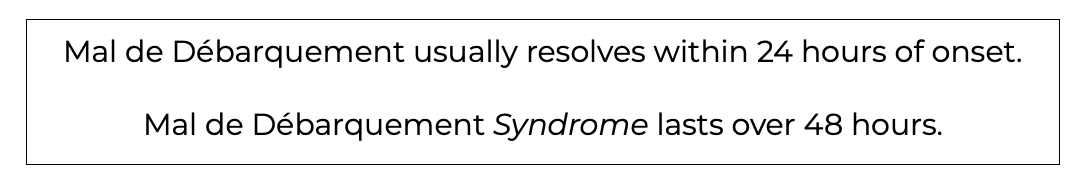
When you get to shore after a long day of boating with the family or friends do you ever feel like you are still in motion despite you are sitting or standing totally still? Then when you move this feeling is less noticeable? This sensation is called Mal de Débarquement and is a normal experience that resolves rather quickly. Mal de Débarquement Syndrome on the other hand presents in a similar manner, but lasts at least 48 hours.
Clinically, at North 49 we never see individuals with Mal de Débarquement, but will see those with Mal de Débarquement Syndrome. In this blog we will cover the 5W’s of Mal de Débarquement Syndrome (MdDS). I must say that Mal de Débarquement Syndrome is one of the vestibular conditions I find the most challenging to treat and from reading this blog you will understand why. So, let’s get started!
WHAT is Mal de Débarquement Syndrome?
MdDS, also known as “Sickness of Disembarkment”, is a neurological disorder of perceived motion. The interesting thing about MdDS is that individuals who have it experience their symptoms when they are not moving, unlike many of the other vestibular disorders that are worse when we move our head or eyes. So, when someone has MdDS they actually feel better while they are in continuous motion such as while being in a moving vehicle (as a passenger or driver).
The earliest known description of MdDS in Western European literature comes from 1689 with William III of Orange who describes how, after crossing the English Channel from the Netherlands to England, the soldiers experienced severe ‘dissiness’ described as, “‘the very Ground seem’d to rowl up and down for some days, according to the manner of the Waves,’.” 1
With Mal de Débarquement Syndrome Here Are Some Of The Common Symptoms:
- A persistent sensation of rocking, swaying, and/or bobbing.
- Difficulty maintaining balance.
- Impaired cognitive function.
- Anxiety and/or depression.
- Fatigue.
- Headache (including migraine).
- Symptom intensity is highly variable among patients and for some can be quite disabling.
- Patients are usually relieved while in motion (i.e. riding in a car). 1-4
Presently, there is no one test that can provide a definitive diagnosis, but it can be diagnosed by a primary care provider, neurologist, or otolaryngologist (ENT) if there is a history of:
- Symptoms or rocking, bobbing, or swaying, etc (non-vertigo); starting immediately after travel by boat, train, plane, or car; that persists for more than 48 hours.
- Feeling of rocking, bobbing, or swaying that improves when the affected person is in continuous motion (i.e. in a moving car).
Along with ruling out other medical problems.1-4
Mal de Débarquement or Vertigo?
If someone has MdDS they will not experience the spinning sensation of vertigo, but rather a rocking, bobbing, or swaying sensation.

WHAT Causes Mal de Débarquement Syndrome?
- Prolonged travel such as long car, plane, or boat trips.
- Being on docks for prolonged periods of time.
- Water beds (do people still have them?).
- Virtual reality.
WHY Does Mal de Débarquement Syndrome Occur?
With prolonged movement your vestibular system simply adapts to the constant motion through neuroplasticity. However, when the body is no longer in motion it takes some time for the vestibular system to recalibrate. Why this takes longer with some people, and why the intensity and duration of symptoms is highly variable remains unknown.
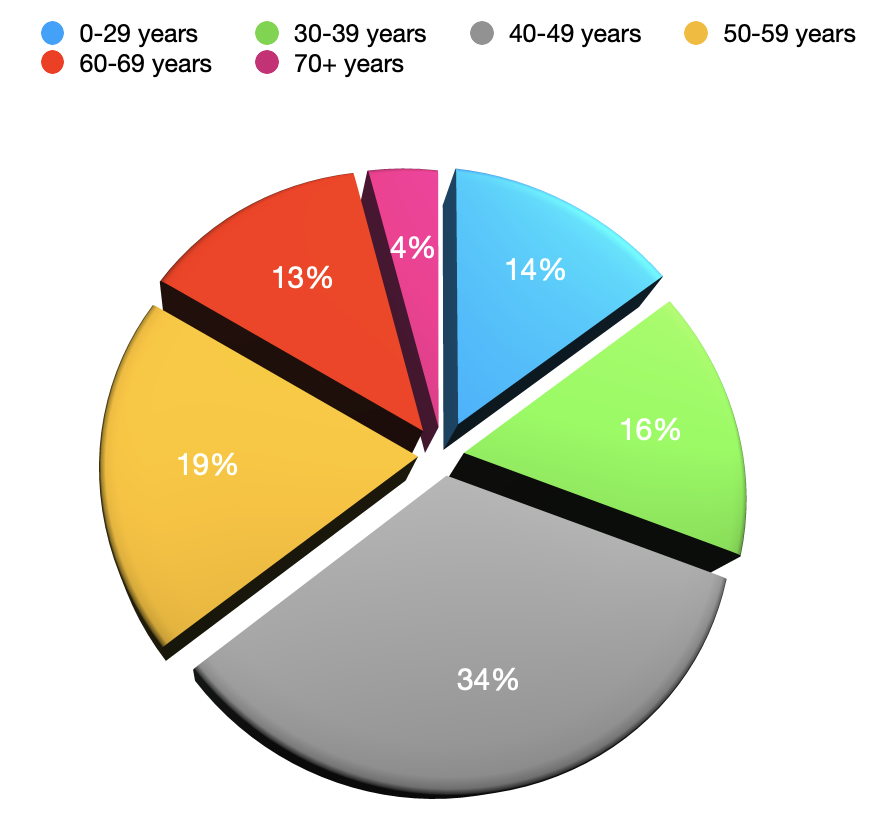
WHO Gets Mal de Débarquement Syndrome?
MdDS is very common with professional sailors, as it is estimated that 75% have experienced it. As we also previously mentioned, anyone who travels can get it, but concurrent physical or psychological stressors as well as hormonal factors can be contributing factors. From the research it seems to affect females more than males and here is a break down of the age categories, with those in their 40’s being the most commonly affected: 2,4
WHEN Does Mal de Débarquement Syndrome Go Away?
As mentioned earlier, the Mal de Débarquement that we experience after a day boating usually goes away rather quickly, typically within 24 hours. Unfortunately for those who develop MdDS, the symptoms can last for days, weeks, months, and even years.
How To Treat Mal de Débarquement Syndrome?
This is where it becomes a challenge as its duration is highly variable and there is no standard treatment approaches. That being said, from research this is what we do know:
- Anticholinergic medications that are beneficial for other forms of dizziness have been found to be non-effective in either treatment or prevention of MdDS.
- There is evidence that benzodiazepines and antidepressants may be beneficial, but they rarely stop the disorder completely.
- In regards to vestibular therapy there are different treatment protocols, but there is a lack of evidence that the symptoms improved with the specific treatment or simply time itself. 5

At North 49 once we have ruled out other sources as the cause for the symptoms, as it is often misdiagnosed, we have found positive results with the following:
- Education and reassurance.
- A gradual re-introduction to the activities that are currently being avoided.
- Addressing lifestyle factors such as caffeine consumption, regular exercise, sleep hygiene, and stress management.
- Working alongside the family physician regarding utilization of the above recommended medications.
- If stress and anxiety are likely key factors, then possible referral to psychology.
Is It Advisable For A Person To Travel If They Have Had Mal de Débarquement Syndrome?
If someone with a history of MdDS plans to travel, there is no telling if the symptoms will reoccur. For some it will not recur and for others the bouts can last longer with each episode. If the symptoms recur the medication mentioned above may help.
To prevent recurrence it may also help to break up long trips to “reset” the vestibular system. Being well rested and stress management are also key.
WHERE Do We Go From Here?
From reading this blog we hope that you get a sense that this is a vestibular condition that is challenging to treat as it is not consistent in who gets it, its intensity, duration, and results with treatment. It is not at all like BPPV that has a consistent history and rapid response to treatment.
That being said, with time we are confident that further research will catch up to what we are experiencing clinically and provide us with an even better understanding of this condition. That way we can have a bigger impact on the quality of life for those affected by it.
For further information about Mal de Débarquement Syndrome feel free to check out the following:
-
- http://www.jvr-web.org/images/ICVD-MaldeDebarquement-Syndrome-DiagnosticCriteria%20Cha-etal.pdf
- https://mddsfoundation.org/wp-content/uploads/2019/05/MdDS-Brochure-2019.pdf
- https://mddsfoundation.org/diagnosing-mdds/
- https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/mal-de-debarquement/
- https://dizziness-and-balance.com/treatment/rehab/MdDs.html